Fatty liver disease affects nearly 25% of adults worldwide, yet many remain unaware until serious complications arise. Often silent in the beginning, this condition can gradually worsen—leading to inflammation, scarring (fibrosis), cirrhosis, and ultimately liver failure if ignored.
However, it’s important to understand that fatty liver is not a permanent condition—it can be reversed.
Your liver is one of the few organs capable of self-repair, and with the right support, it can bounce back. By making key lifestyle and nutritional changes, you can reduce liver fat, restore function, and significantly lower the risk of long-term damage—without the need for harsh medications or invasive treatments.
This article presents six powerful, natural strategies proven to support liver healing. Whether you’re in the early stages of fatty liver or facing more advanced challenges, these methods can help you turn your health around—starting today.
⚠️ Disclaimer:
The information provided in this article is for educational and informational purposes only. It is not intended as medical advice or a substitute for professional healthcare. Always consult with your doctor or a qualified healthcare provider before making any changes to your diet, lifestyle, or supplement routine—especially if you have a pre-existing liver condition or if you are on medication.
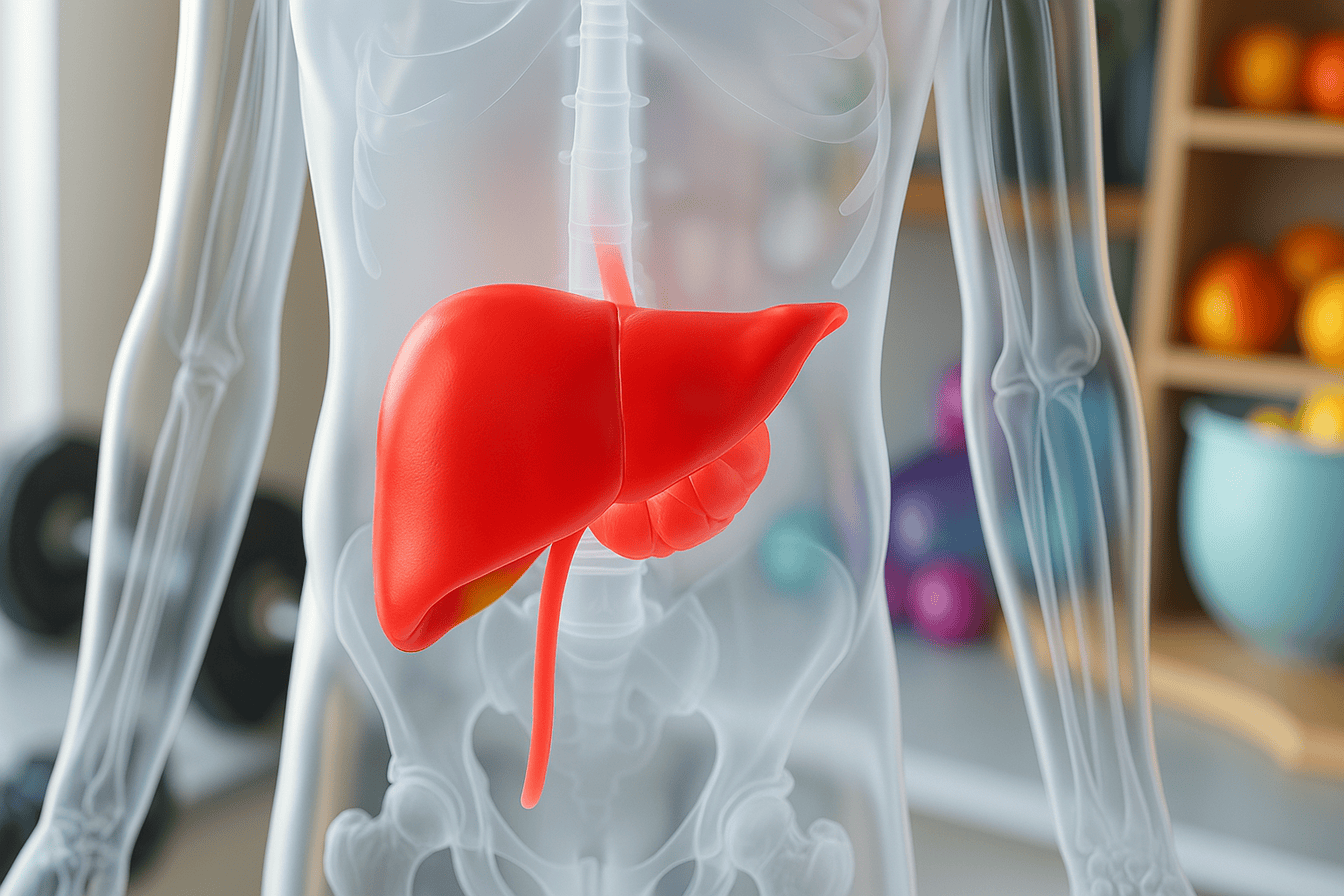
Understanding the Progression of Fatty Liver Disease
Fatty Liver is a Spectrum—Know Where You Stand
Liver disease does not develop overnight; it progresses through stages that often remain asymptomatic, earning it the nickname “the silent disease.”
The Four Key Stages:
- Steatosis (Fatty Liver): Early stage; fat accumulates in liver cells.
This state is the earliest and most commonly observed stage of liver disease. Fat begins to accumulate in liver cells, typically as a result of poor diet, insulin resistance, or a lack of physical activity. At this stage, the liver continues to function normally, and there is no inflammation or scarring, which means the condition is still reversible.
- Non-Alcoholic Steatohepatitis (NASH): Inflammation occurs, and liver enzymes elevate.
At this stage, the situation becomes more serious. In addition to fat accumulation, the liver experiences inflammation, and liver cells may start to deteriorate. Blood tests frequently reveal elevated liver enzymes. Without proper intervention, this stage can lead to permanent damage.
- Fibrosis: Scar tissue begins to replace healthy tissue.
The liver starts to form scar tissue in response to ongoing inflammation. While healthy liver tissue still exists, it’s being replaced by fibrous tissue, making it harder for the liver to function efficiently. This stage is still potentially reversible with the right lifestyle changes.
- Cirrhosis: Severe scarring disrupts liver function, often considered irreversible.
This level is the most advanced stage. The liver becomes severely scarred and hardened, and normal function is significantly impaired. At this point, damage may be permanent, and the risk of liver failure or cancer increases. Often, a liver transplant may be required.
Visible Warning Sign: Belly Fat
Carrying a lot of belly fat, especially visceral fat around your organs, increases the likelihood of liver damage. Could you perform a simple test? If you look down and can’t see your toes because of your belly, your liver is likely storing excess fat.
The 6 Most Effective Ways to Heal a Fatty Liver
1. Activate Autophagy: Your Body’s Internal Reboot Mechanism
One of the most powerful tools your body has to clean and repair itself is a process called autophagy.
The word autophagy comes from Greek, meaning “self-eating.” While that might sound scary, it’s a natural, healthy process where your body breaks down old, damaged, or unnecessary cells and recycles their parts to build new, healthier ones.
Think of it like spring cleaning at the cellular level—especially important when your liver is overwhelmed with fat, toxins, or inflammation.
How Autophagy Supports Liver Healing
When activated, autophagy helps the liver by:
- Breaking down fibrotic (scar) tissue, which is key to reversing damage
- Detoxifying damaged or malfunctioning cells, improving liver performance
- Clearing out damaged mitochondria, which are linked to many chronic diseases
- Removing viruses, bacteria, and yeast that may be hiding in liver cells
- Modulating the immune system, especially useful in autoimmune liver conditions
It’s your body’s way of saying, “Let me clear out the junk so we can start fresh.”
How to Trigger Autophagy Naturally
Autophagy doesn’t happen when you’re constantly eating or snacking. It kicks in when your body goes into a rest-and-repair state—usually when food is not being digested.
Here are proven ways to activate autophagy:
- Intermittent Fasting (like the 18:6 or 20:4 method): Eat within a set time window and fast the rest of the day.
- Extended Fasting (48–72 hours occasionally): More intense but powerful for deep cellular clean-up.
- Exercise (especially high-intensity or resistance training): Physical stress encourages the body to recycle old cells.
- Quality Sleep (7–8 hours of uninterrupted rest): Autophagy is naturally boosted during deep sleep cycles.
- Cold therapy and saunas: These create mild stress responses (called hormesis), which stimulate healing and cell renewal.
- Dietary support: Cruciferous vegetables (like broccoli and kale), extra virgin olive oil, and even moderate coffee intake can encourage autophagy.
“Autophagy is the body’s best natural detox—it’s free, effective, and regenerative.”

2. Fasting: The Most Powerful Tool to Reduce Liver Fat
While many people associate fasting with weight loss, its benefits go much deeper—especially when it comes to healing your liver. Fasting gives your body a break from constant digestion, allowing it to focus on repair, detoxification, and fat burning, including the fat that accumulates inside the liver.
When you fast, your insulin levels drop, your body starts using stored fat for energy, and your liver gets a chance to offload the toxic burden it’s been carrying.
Why Fasting Heals the Liver
Fasting supports liver repair and fat reduction in several powerful ways:
- Lowers insulin resistance: High insulin levels are a major driver of a fatty liver. Fasting helps restore insulin sensitivity so your liver can function properly again.
- Decreases triglycerides and liver enzyme levels: These are common markers of liver stress. Regular fasting can bring them back to healthy ranges.
- Regenerates mitochondria: Your liver’s energy-producing engines (mitochondria) often become damaged. Fasting stimulates the creation of new, healthier cells.
- Activates antioxidant pathways (like Nrf2): Fasting naturally boosts your body’s internal defense system, helping to neutralize oxidative stress that damages liver cells.
Beginner Tips for Fasting Safely
If you’re new to fasting, start slow. Fasting doesn’t mean starving—it means giving your body structured time to heal.
Here’s how to begin:
- Start with 12–14 hour fasts: Try not eating from dinner until late breakfast or lunch. Gradually increase to 16 or 18 hours if it feels good.
- Stay hydrated: Drink plenty of water and consider adding electrolytes (like a pinch of sea salt or magnesium) to support energy and prevent fatigue.
- Break your fast wisely: When it’s time to eat, start with nutrient-dense, low-carb meals—like leafy greens, healthy fats, and protein—to avoid spiking blood sugar.
- Avoid snacking between meals: This keeps insulin levels low and gives your liver more recovery time.
“Fasting isn’t starvation—it’s structured nourishment for liver healing.”
3. TUDCA: The Bile Salt That Repairs Liver Cells
TUDCA (Tauroursodeoxycholic Acid) is a naturally occurring bile acid your liver produces to help digest fats. But TUDCA is much more than just a digestive aid.
It plays a crucial role in protecting and repairing liver cells, improving bile flow, and reducing inflammation and scarring—making it especially useful for people with fatty liver, cholestasis, or cirrhosis.
While it’s been used in traditional medicine for thousands of years (particularly in Chinese medicine), modern research has confirmed that TUDCA has powerful liver-healing properties.
TUDCA Benefits for Fatty Liver and Cirrhosis
Here’s what makes TUDCA such a valuable addition to your liver-healing protocol:
- This bile prevents cholestasis and gallstone formation: Thick or sluggish bile can back up in the liver, causing damage. TUDCA helps keep bile flowing smoothly.
- Reduces inflammation in bile ducts: Inflammation can block bile ducts and trigger scarring—TUDCA calms this inflammation and promotes flow.
- Regenerates hepatocytes (liver cells): TUDCA directly supports the repair and regeneration of liver tissue damaged by fat or fibrosis.
- Protects against oxidative damage: It acts as a shield for liver cells under stress from toxins, alcohol, or medications.
- Decreases fibrosis and scar tissue: Regular use of TUDCA has been shown to help reduce liver stiffness and break down early-stage scarring.
Optimal TUDCA Usage
To get the most benefit from TUDCA:
- Take 2 capsules on an empty stomach, once in the morning and again in the afternoon.
- Avoid taking it with meals, as it will primarily help digest food instead of targeting liver repair.
“TUDCA is one of the most underrated yet effective tools for advanced liver healing.”
4. Boost Phase 1 and 2 Liver Detoxification
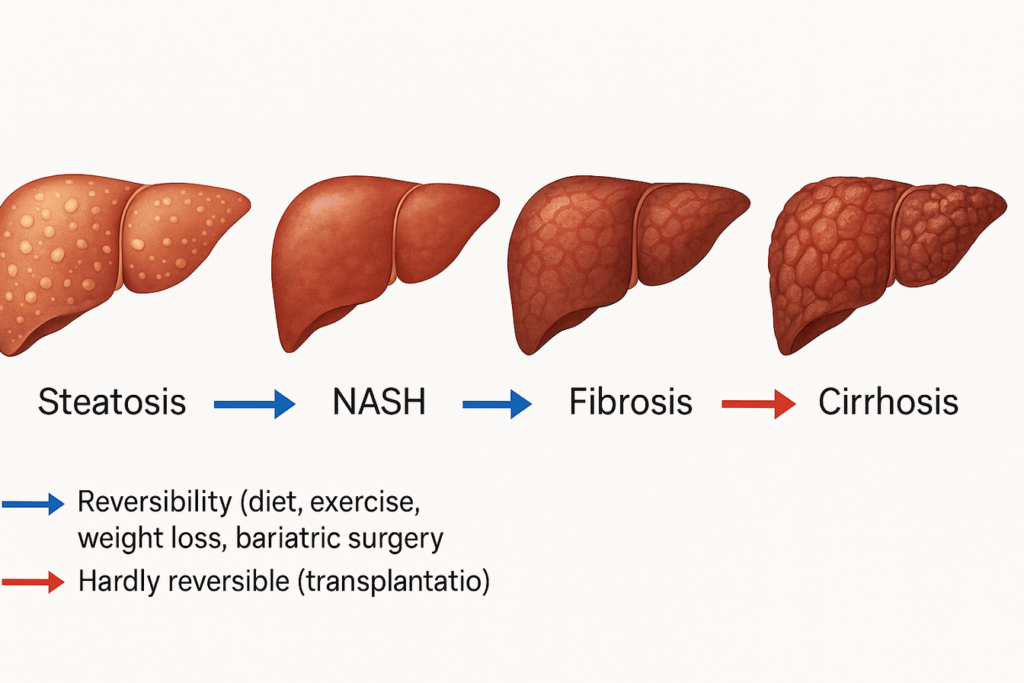
Your liver is the body’s central detox hub. Every day, it filters blood, breaks down toxins, metabolizes hormones, and processes everything from alcohol to medications. To do its job effectively, it relies on a two-phase detoxification process that must stay in balance.
Understanding the Two Detox Phases
- Phase 1: Activation
In this phase, the liver uses enzymes to break down toxins—like pesticides, alcohol, medications, or chemicals—into smaller particles. These particles are often more reactive and dangerous, so the next phase must kick in quickly to neutralize them. - Phase 2: Conjugation & Elimination
Here, the liver binds these activated toxins to protective compounds like sulfur, glutathione, or amino acids, making them water-soluble. Once converted, the body can safely excrete them through urine, sweat, or bile.
If either phase is sluggish, toxins can accumulate and circulate back into your bloodstream, increasing inflammation and damaging liver cells.

Best Foods to Support Liver Detoxification
Nature offers many foods that can support both detox phases, especially Phase 2, which is often the weakest link.
Here are some of the most effective liver-detox-supporting foods:
- Broccoli sprouts—rich in sulforaphane, a powerful compound that boosts both Phase 1 and Phase 2 enzymes
- Cruciferous vegetables (like cabbage, Brussels sprouts, and kale) Help activate detox enzymes and provide sulfur for conjugation
- Green tea—Contains catechins, antioxidants that enhance liver enzyme activity and reduce inflammation
- Radishes and arugula—packed with glucosinolates, which support detox and bile flow
- Onions and garlic—High in sulfur compounds that fuel glutathione production, your body’s master detoxifier
These foods don’t just help detox the liver—they also nourish and protect it, making them essential in any liver-healing diet.
“Food is the first line of defense in liver detox—not pills.”
5. Milk Thistle: The Most Researched Herbal Liver Protector
Milk thistle (Silybum marianum) is one of the most studied and trusted natural remedies for liver health. Used for over 2,000 years in traditional medicine, it’s now backed by modern research for its ability to protect, heal, and regenerate liver cells.
The key active compound in milk thistle is silymarin, a group of flavonoids that act as antioxidants, anti-inflammatories, and liver cell protectants. Whether your liver is burdened by fatty accumulation, inflammation, or toxins from medications and alcohol, milk thistle offers a natural defense.
Milk Thistle Liver Benefits
Here’s how milk thistle supports your liver’s healing process:
- Protects against toxic liver damage: Shields liver cells from harmful substances like alcohol, medications (e.g., acetaminophen), and environmental toxins.
- Reduces liver inflammation: Helps calm the immune response and lowers inflammatory markers that contribute to disease progression.
- Stimulates cell regeneration: Encourages new hepatocyte (liver cell) growth, helping replace damaged tissue.
- Lowers ALT & AST enzymes: These enzymes, elevated in liver damage, often normalize with milk thistle supplementation.
- Detoxifies alcohol, medications, and heavy metals: Supports both detoxification phases while reducing oxidative stress.
Bonus Healing Power
Milk thistle is so potent it has even been used in hospitals to counteract poisoning from death cap mushrooms, which are otherwise fatal due to their liver-destroying toxins.
It’s also helpful for people taking long-term medications that strain the liver. Whether it’s cholesterol meds, painkillers, or antidepressants, adding milk thistle may help reduce side effects and protect the liver.
“Milk thistle is a liver’s best herbal ally—it protects and repairs at a cellular level.”
6. Tocotrienols: The Liver-Saving Form of Vitamin E
Tocotrienols are a lesser-known but highly potent form of vitamin E, and they’re quickly gaining recognition as one of the most promising nutrients for liver health. While most people are familiar with tocopherols (the common form of vitamin E found in supplements), tocotrienols have an entirely different and more powerful effect—especially when it comes to reducing liver inflammation and fibrosis.
These compounds are incredibly effective at protecting liver cells from damage, reversing early stages of scarring, and enhancing the liver’s ability to heal itself.
Why Tocotrienols Matter
Here’s how tocotrienols can make a real difference in fatty liver and liver disease recovery:
- Break down liver scar tissue: They help soften and reduce existing fibrosis, allowing liver tissue to regain flexibility and function.
- Prevent new fibrosis formation: Tocotrienols disrupt the scarring process, effectively stopping disease progression.
- Lower oxidative stress: As powerful antioxidants, they neutralize free radicals that would otherwise damage liver cells.
- Reduce risk of liver cancer: Long-term liver inflammation and fibrosis can lead to cancer—tocotrienols may reduce this risk through cellular protection and immune modulation.
- Support healthy lipid profiles: They help manage cholesterol and triglycerides, which are often elevated in those with fatty liver.
Usage Tip
To get the full benefits, always choose a pure tocotrienol complex—not mixed with tocopherols, as the two forms can compete for absorption and reduce effectiveness.
Look for annatto-based tocotrienols, which are considered among the most potent and pure forms available.
“Tocotrienols are your secret weapon in reversing fibrosis and protecting your liver for life.”
Common Causes of Liver Damage You Can Avoid
While lifestyle changes and natural remedies can help heal your liver, it’s just as important to understand what may be damaging it in the first place. Many people are unknowingly exposing their liver to stressors that, over time, can lead to fatty liver, fibrosis, or even cirrhosis.
Here are some of the most common (and often overlooked) causes of liver damage—and what you can do about them.
1. High Iron Levels (Hemochromatosis)
Excess iron in the body can lead to a condition called hemochromatosis, where iron builds up in the liver and other organs, causing inflammation and scarring. This disorder is often genetic but can also result from taking too many iron supplements without monitoring.
🩺 Tip: Ask your doctor to check your serum ferritin and transferrin saturation levels if you suspect high iron or experience fatigue, joint pain, or abdominal discomfort.
2. Blocked Bile Ducts (Gallstones, Infection)
Your liver produces bile to digest fats, and that fluid flows through ducts to the gallbladder and intestines. When these ducts become blocked by gallstones or infection, bile backs up into the liver, causing irritation, inflammation, and, over time, damage.
Signs may include upper right abdominal pain, jaundice (yellowing of the skin), or digestive issues after eating fatty meals.
3. Autoimmune Liver Conditions
Occasionally, the immune system mistakenly attacks liver tissue, leading to chronic inflammation and damage. This category includes conditions like autoimmune hepatitis, primary biliary cholangitis (PBC), and primary sclerosing cholangitis (PSC).
These are often underdiagnosed, especially in women, and may present with fatigue, itchy skin, or elevated liver enzymes.
4. Alcohol, Tylenol, and Medication Overuse
Alcohol is one of the most well-known liver toxins, but many people don’t realize that over-the-counter medications like acetaminophen (Tylenol) can be just as damaging in large or frequent doses. Long-term use of prescription medications, especially statins, antibiotics, and anti-inflammatories, can also strain the liver.
Pro Tip: If you take medications regularly, consider supporting your liver with natural protectants like milk thistle and N-acetylcysteine (NAC) under the guidance of a healthcare provider.
5. Nutrient Deficiencies
Your liver relies on specific nutrients to function optimally—especially those involved in fat metabolism and detoxification.
Key deficiencies that impair liver health include:
- Vitamin D—Vital for immune function and inflammation control
- Magnesium—Helps regulate enzymes and detox pathways
- Choline—Crucial for transporting fat out of the liver
A poor diet, chronic stress, or certain medications can deplete these nutrients, making liver healing harder.
Pro Tip:
Consider getting routine liver function tests (ALT, AST, GGT), a ferritin panel, and even a liver ultrasound if you’re experiencing symptoms like fatigue, abdominal bloating, or unexplained weight gain.
The earlier you detect imbalances, the easier it is to reverse them.
Conclusion: Take Control of Your Liver Health Today
You don’t have to live with fatty liver disease forever. In fact, with the right knowledge and actionable steps, it can be prevented, managed, and, often, reversed—even in the later stages like fibrosis or early cirrhosis. Your liver is one of the most resilient organs in your body, capable of regenerating itself, but only if you give it the support it needs.
You now have a comprehensive toolkit to begin your healing journey, including powerful lifestyle interventions like intermittent and prolonged fasting, nutrient-dense liver-supportive foods, and science-backed supplements such as TUDCA, milk thistle, and tocotrienols. These strategies don’t just reduce fat in the liver—they actively promote cellular repair, reduce oxidative stress, improve bile flow, and protect against further damage.
What makes liver health even more critical is that it’s connected to nearly every other function in your body—hormone regulation, digestion, detoxification, energy metabolism, and even immune defense. A sluggish or damaged liver can contribute to fatigue, weight gain, brain fog, poor digestion, skin issues, and a weakened immune response.
Consistency is key when it comes to healing your liver. This process won’t happen overnight, but every step you take—whether it’s fasting, eating healthy meals, or taking targeted supplements—will bring you closer to restoration and vitality. Even minor improvements in liver function can lead to significant boosts in energy, mental clarity, and overall wellness.
If you’re seeking to prevent liver disease, reverse fatty liver, or support liver regeneration after years of damage, your efforts are worthwhile. Your body can heal; it just needs the right environment and your commitment to the process.
Start now. Take the first step. Your liver—and your future self—will thank you.
⚠️ Disclaimer:
The information provided in this article is for educational and informational purposes only. It is not intended as medical advice or a substitute for professional healthcare. Always consult with your doctor or a qualified healthcare provider before making any changes to your diet, lifestyle, or supplement routine—especially if you have a pre-existing liver condition or if you are on medication.
📚 References & Further Reading
1. Fatty Liver Disease Overview
https://medlineplus.gov/fattyliverdisease.html
2. Cleveland Clinic—Nonalcoholic Fatty Liver Disease (NAFLD)
https://www.ccjm.org/content/89/12/719
3. WebMD—Fatty Liver Disease: What to Know
https://www.webmd.com/fatty-liver-disease/fatty-liver-disease
4. PMC-—PubMed Central/National Library of Medicines
https://pmc.ncbi.nlm.nih.gov/articles/PMC8958240
5. PubMed—Effects of Milk Thistle on Liver Health
https://pubmed.ncbi.nlm.nih.gov/12427501
6. Examine.com—TUDCA Supplement Overview
https://examine.com/supplements/tudca/?show_conditions=true
7. Clinical Education: Role of Tocotrienols in Liver Fibrosis